Hyperbaric Medicine
Hyperbaric oxygen therapy can expedite the healing of certain types of chronic, non-healing wounds, such as diabetic wounds, as well as reduce patient suffering, disability and prevent unnecessary hospitalizations and amputations.
Hyperbaric Oxygen Therapy (HBOT) is recognized by Health Canada, all provincial Ministries of Health and internationally for of the following conditions:
- Decompression sickness
- Air or gas embolism
- Arterial Insufficiencies:
- Selected Problem Wounds
(Diabetic ulcers) - Central Retinal Artery Occlusion
(sudden blindness)
- Selected Problem Wounds
- Osteomyelitis (bone infections)
- Delayed Radiation Injuries
- Compromised grafts and flaps
- Sudden hearing loss
- Crush injuries
- Acute thermal burns
- Carbon monoxide poisoning
- Gas gangrene
- Necrotizing soft tissue infections
(flesh-eating disease) - Severe anemia
- Intracranial abscess
- Avascular Necrosis (Aspectic Osteonecrosis – hip)
Hyperbaric Oxygen: How it works
Blood is comprised of red blood cells, containing hemoglobin and serum, a clear, colourless fluid. Oxygen is normally transported to the tissues by the red blood cells, by attaching to the hemoglobin. In patients with severe atherosclerosis and blood vessels partially or fully occluded by plaque, passage of red blood cells may be blocked. This results in tissue ischemia (lack of blood) and hypoxia (lack of oxygen). Hyperbaric oxygen therapy saturates both the red blood cell hemoglobin and the serum with oxygen. Oxygen saturated serum can traverse some of these occluded vessels and supply badly needed oxygen to these tissues. While in a hyperbaric chamber, oxygen saturated serum can support life, even in the absence of hemoglobin. Patients with severe anemia (blood loss and/or low hemoglobin) can be successfully kept alive in a hyperbaric chamber until matched blood becomes available.
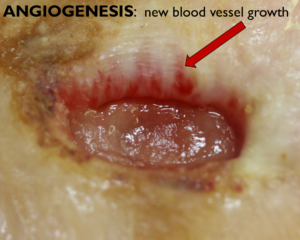
In tissues that have poor circulation, ischemia (lack of blood) and/or hypoxia (lack of oxygen), the macrophages (cells that fight infection) and fibroblasts (cells responsible for wound healing) cannot function. Wounds can deteriorate and ultimately may result in limb amputation. Hyperbaric oxygen can arrest and reverse this situation by causing angiogenesis, the growth of new blood vessels, as shown in the following macro-photograph of a healing wound.
Hyperbaric oxygen increases the release of nitric oxide, which in turn causes the release of stem cells, which differentiate into blood vessels, skin and nerve cells. A single hyperbaric treatment can double the amount of circulating stem cells. After twenty or more hyperbaric treatments, stem cells can be increased eightfold.
Hyperbaric oxygen also causes the release of growth factors in the blood including:
- Vascular Endothelial Growth Factor (VEGF)- binds to blood vessel walls causing new blood vessels growth
- Platelet Derived Growth Factor (PDGF) – regulates cell growth, division and angiogenesis
- Matrix Metallo-Proteinase (MMP- 2 & 9) – increases tissue remodelling and angiogenesis
- Tissue Inhibitor of Metallo- Proteinase (TIMP-1) – promotes cell proliferation
In addition, hyperbaric oxygen:
- Bactericidal/static (kills/suppresses) many of the bacteria responsible for wound infections, including those bacteria responsible for gas gangrene and necrotising fasciitis (flesh eating disease)
- Decreases the ischemia/Reperfusion injury often seen in crush injuries
- Decreases the lipid peroxidation injury in carbon monoxide poisoning which can result in irreversible brain damage.
- Saves failing skin grafts and flaps
Note:
Topical oxygen therapy is not hyperbaric therapy and the two treatments should not be confused. Linden R, Ledez K, Hopf H, Fife C. Int Wound J. 2014 Apr;11(2):230-1. doi: 10.1111/j.1742-481X.2012.01069.x. Epub 2012 Aug 22.PMID: 22913614
 Hyperbaric Oxygen
Hyperbaric Oxygen